Intake, Extract, and Validate
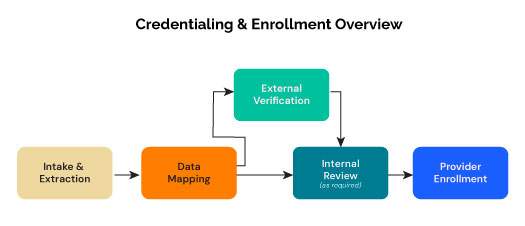
The goal of our intelligent, automated platform is to streamline provider enrollment form filling and credentialing across multiple payer portals, eliminating manual processing inefficiencies and reducing errors through AI-powered automation. By using agents for data mapping, review, and enrollment, the entire process should result in greater than 95% accuracy without the need for any manual intervention.
Like all automation and AI processes, human-in-the-loop steps are included to ensure the highest levels of accuracy and strictest adherence to compliance.