OnDemand Prior Authorization Webinar
How is AI redefining Prior Authorization—and what should payers be doing now to prepare?
Overview
 Join a panel of seasoned healthcare and automation experts from Genzeon and UiPath as they unpack the critical challenges and emerging opportunities in Prior Auth transformation. This forward-looking session is crafted for payer leaders navigating evolving regulatory demands, operational bottlenecks, and the push toward intelligent automation.
Join a panel of seasoned healthcare and automation experts from Genzeon and UiPath as they unpack the critical challenges and emerging opportunities in Prior Auth transformation. This forward-looking session is crafted for payer leaders navigating evolving regulatory demands, operational bottlenecks, and the push toward intelligent automation.
Together, they’ll explore:
- Strategic approaches to full-spectrum prior authorization automation
- Navigating the intersection of policy, regulation, and innovation
- Realistic applications of AI-driven workflows in payer operations
- Case insights into how leading organizations are preparing for CMS-mandated changes
The session will also provide a behind-the-scenes look at how Genzeon’s Agentic AI approach—combined with UiPath’s Applied AI platform—is helping payers enhance compliance readiness, streamline approvals, and achieve measurable ROI.
Whether you’re in the early stages of your automation roadmap or already executing AI initiatives, this conversation offers practical insights and frameworks you can act on immediately.
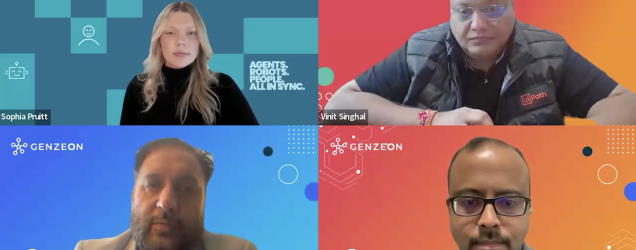
Speakers
- Sophia Pruitt, Senior Solutions Engineer at UiPath
- Vinit Singhal, Payer Strategy Lead at Genzeon
- Harsh Singh, General Manager, Healthcare at Genzeon
- Prashant Krishnakumar, AI & Automation Practice Lead at Genzeon
Frequently Asked Questions
Prior authorization (PA) is a process used by payers to determine whether a prescribed procedure, service, or medication will be covered under a member’s plan. It is intended to ensure medical necessity, avoid unnecessary costs, and improve patient safety. Manual PA processes are often time-consuming, leading to care delays, administrative burden, and increased costs for both payers and providers.
Traditional PA workflows often involve manual and analog work: data entry, faxes, phone calls, and back-and-forth communication between providers and payers. These inefficiencies cause delays in patient care, high operational costs, inconsistent decision-making, and administrative burnout. In some cases, errors in documentation or incomplete submissions lead to denials, unnecessary appeals, and further delay.
Yes. Modern PA automation solutions are designed to meet strict regulatory and security standards, including HIPAA compliance for handling protected health information (PHI). Many solutions include audit trails, configurable policy rules, and real-time reporting capabilities to ensure transparency and adherence to payer guidelines and government regulations, such as those outlined by CMS (Centers for Medicare & Medicaid Services). AI Governance is vitally important however to ensure continued compliance.