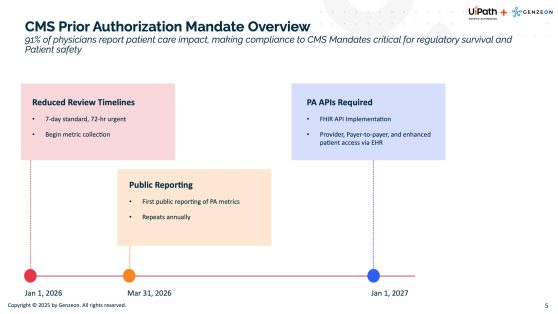
CMS mandates begin in January 2026.
CMS has finalized rules (e.g., CMS-0057-F) requiring payers to streamline prior authorization processes.
Key changes include tighter response times, transparency requirements, and mandated adoption of standardized APIs for electronic submission and status tracking. See the matching graphic for more information on these deadlines.